#ICEM2025 May 26th Recap!
- Shahbaz Syed

- May 26
- 43 min read
Updated: May 28
Monday delivered another full day of learning and connection, kicking off with a packed plenary session, hands-on educational workshops, and a wide range of engaging concurrent tracks. The day wrapped up in style with the much-anticipated Welcome Gala and a crowd-favorite performance by Docs That Rock!
To read more in depth on the concurrent sessions - click on the dropdown arrow!
🌟 Plenary Session One: Toxic Leadership in Healthcare – How Difficult Doctors Undermine Team Performance.
Speaker: Dr. Victoria Brazil
Bottom Line:
Toxic leadership in healthcare isn’t always someone else’s problem - it’s a cultural issue that affects team performance, patient outcomes, and clinician retention. Building high-functioning teams starts with self-reflection, structured feedback, and collective accountability.
The Case That Hits Too Close to Home
Dr. Victoria Brazil opened with a case many of us know all too well: a straightforward pancreatitis presentation that quickly descends into a fragmented, frustrating phone call to a specialty service. The patient needs admission, but between the curt tone, the contradictory messages, and the eventual hang-up, it’s clear that poor communication and toxic interprofessional dynamics are compromising care.
It’s easy to blame “the other doctor on the phone.” But then she flips the script.
A second moment: a bright-eyed medical student’s first day. The attending’s response?
“Hey mate… that’s my chair.”
We’ve all worked with difficult doctors. But have we ever been the difficult one?
Psychological Safety and Emergency Medicine
This study demonstrated that psychological safety, the belief that team members can speak up without fear is a critical determinant of team performance in the ED.
Trainees reported EM as progressive and non-hierarchical, but nursing staff identified ongoing concerns about arrogance and lack of respect from physicians.
Bad Behaviour: An Insidious Threat
Key Article: Bad Behaviour in Healthcare: A Threat to Patient Safety, Staff Wellbeing, and Organizations (Crowe, Riley)
Unprofessional behaviour in clinical teams undermines morale, increases burnout, and is linked to higher turnover and worse patient outcomes.
The ripple effect of toxic leadership reaches every corner of the system, especially in high-stakes environments like emergency care.
Culture Change Through Teamwork
Dr. Brazil emphasized that high-performing teams are built intentionally, and that change starts from within the team itself.
She shared examples from the High Performance Clinical Teamwork Strategy (2022–2023):
This initiative focused on improving team behaviours and shared culture across disciplines to enhance performance under pressure.
Programs included large-scale simulations in trauma, obstetrical hemorrhage, and the NICU, reinforcing inter-team communication and collaboration.
The unifying message: “Team behaviours shape outcomes.” And at the core of those behaviours are beliefs and attitudes that can be shaped through structured reflection and mutual accountability.
Simulation, Debriefing, and Culture Building
Through regular team debriefs, clinicians reflected on their expectations of one another and how they wanted to function as a team. Notably, participants emphasized how respectful communication between specialties, modeled and reinforced during simulation - translated to better collaboration in actual emergencies.
One example: improving obstetrical hemorrhage outcomes through interdisciplinary simulation fostered stronger inter-team relationships, which over time led to measurable clinical improvements.
What Can We Do Tomorrow?
Culture change doesn’t require a committee or a policy — it starts with small, consistent actions. As Dr. Brazil highlighted, two of the most modifiable factors for improving team performance are:
Leader behaviours
Team familiarity
Even something as simple as a pre-brief or post-shift debrief can shape how a team communicates and collaborates. Individual actions matter — not just in how we perform, but in how we build a culture that lifts everyone up.
Takeaways
Talk with your teams about expectations, normalize the conversation.
Be an upstander, address poor behaviour constructively and support colleagues in real time.
Look in the mirror, acknowledge when you may have contributed to toxicity, and commit to growth.
As Dr. Brazil reminded us: “We often think in silos, but patients are cared for by teams — and teams thrive on culture.”
📝 Plenary Session Two: Hybrid Warfare and a New Era of Mass Casualty Response
Speaker: Dr. Eveline Hitti
Bottom Line:
Mass casualty events are no longer isolated to war zones. In a world marked by instability and rising global conflict, emergency departments must prepare for mass trauma on an unprecedented scale. Scalable, hospital-wide protocols and rapid activation systems are now critical to emergency preparedness.
A Career Shaped by Conflict
Dr. Eveline Hitti did not begin her career with an interest in disaster medicine. But growing up in civil war-era Lebanon, training in Baltimore, and eventually returning to help build academic emergency medicine in her home country, she found herself thrust into a world where mass casualty response became routine.
In 2013, a car bombing near her hospital resulted in 37 casualties arriving at once. Over the next six years, she led the response to 12 mass casualty events. From this experience, her team developed a rapid protocol known as the “golden 15 minutes” — a critical window in which to mobilize staff, secure the department, begin triage, and activate surge capacity before losing operational control.
August 4, 2020 – A Catastrophic Turning Point
The Beirut Port explosion changed everything. With 2.7 tons of ammonium nitrate detonating just kilometers from her hospital, the injuries were on a different scale — including among hospital staff and family members. Institutional protocols designed for earlier mass casualty incidents proved insufficient.
This tragedy led to a fundamental shift in their approach: mass casualty response had to move beyond the emergency department and become hospital-wide.
Scaling Up: Moving From ED-Focused to Hospital-Based Response
Dr. Hitti emphasized the need to engage the entire hospital — from medicine and pediatrics to surgical subspecialties — in disaster preparedness. This meant:
Training non-EM staff in basic trauma and mass casualty care
Developing secondary triage protocols for identifying patients who could be stabilized and transferred to inpatient units
Establishing systems to offload the ED rapidly and maintain capacity
This shift was put to the test on September 17, 2024, during a coordinated attack in which explosive devices were hidden in pagers. With over 180 patients arriving in just hours, many with complex facial, hand, and ocular injuries, the team had to scale their response immediately.
Key Challenges in Modern Mass Casualty Events
Triage and Patient Flow
Secondary triage systems were used to identify stable patients without torso injuries for early transfer upstairs, often within 20 minutes of arrival.
Imaging Bottlenecks
With dozens of CT scans needed urgently, imaging became a limiting factor. The team used point-of-care ultrasound and physician-led prioritization to manage the flow.
Surgical Capacity
In the first 12 hours, 35 patients required surgery, many for specialized procedures. Prioritization was handled dynamically, often within the OR itself.
National Health System Coordination
The response quickly exceeded institutional capabilities. Hospitals across the country delayed elective surgeries and mobilized to support the surgical and supply demands of specialized care.
Psychological and Structural Impacts
Beyond the immediate medical response, there were significant secondary effects:
Pervasive psychological trauma among victims and providers
Disrupted communication systems, as pagers were no longer trusted
Strain on healthcare infrastructure, with long-term implications for continuity of care
This pattern, described as hybrid warfare, involves not only physical attacks but also the targeted disruption of healthcare infrastructure, communication, and public trust.
Lessons From the Frontline
Dr. Hitti’s message was clear: in an era of global instability, every healthcare system must be ready for mass casualty events. Hybrid warfare is no longer theoretical. It threatens not only the acute care response, but also long-term access to care for chronic illness, elective surgery, and essential medication.
A Message of Endurance
Dr. Hitti closed with a deeply personal reflection on her 15 years in Lebanon, and the strength she draws from colleagues working under immense pressure in conflict zones.
“In times of uncertainty, two things are certain. This moment will pass, and we will live with the decisions we made during the crisis. May we all reach the other end knowing we did all that we could.”
🧠 Educational Marketplace
The Educational Marketplace at ICEM 2025 offered a dynamic, hands-on space where emergency medicine educators, innovators, and learners came together to share, explore, and inspire. With stations representing institutions and organizations from around the world, the marketplace celebrated diversity in educational strategy, creativity in delivery, and commitment to global collaboration.
From low-fidelity simulation models and procedural trainers to digital learning platforms, visual case-based tools, and open-access curricula, the exhibits highlighted practical, scalable, and globally relevant innovations in emergency medicine education.
Key themes included:
Equity in access to training materials and educational design
Interprofessional collaboration and team-based learning
Digital scholarship, FOAMed tools, and asynchronous education models
Culturally contextualized curricula for low-resource and rural settings
Above all, the Marketplace embodied the spirit of ICEM: building bridges between continents, disciplines, and ideas — and reminding us that education is not just content delivery, but connection

🔍 Morning Concurrent Tracks
EMS: Presentations focused on pre-hospital care innovations, including community paramedicine programs and strategies for improving response times.
Speakers: Dr. Daniel Beamish, Dr. Connor Ingles, Shannon Leduc, Robert Leduc
Empowering Paramedics to Rethink 911: Supporting New Models of Prehospital Care and Enhanced ED Diversion
The traditional 911 model assumes every call signals a medical emergency requiring ED transport. But in practice, many patients calling 911 are low acuity, often not requiring hospitalization at all. In Ottawa, this disconnect contributes to severe offload delays, with 100,000 hours of paramedic time lost annually — equivalent to 47 full-time paramedics per day.
This team developed a novel prehospital care model aiming to reduce unnecessary ED visits by empowering paramedics to safely identify and divert low-acuity patients away from the emergency department.
Key Elements of the Program:
Targeted paramedic training in low-acuity triage, frailty scoring, and shared care planning
Mentorship from emergency physicians through case-based classroom sessions
24/7 Online Medical Consultation to guide real-time triage decisions
Follow-up by community paramedics within 24 hours for safety, satisfaction, and referral.
Results:
590 patients diverted from the ED
95% reported stable or improved symptoms
Only 3.2% re-accessed 911 within 72 hours
94% felt safe staying at home
91.5% were satisfied or very satisfied with the care they received

Bottom Line:
This model demonstrates that low-acuity patients can be safely triaged by paramedics, supported by targeted training, infrastructure, and physician consultation. The program reduced ED burden, improved patient experience, and delivered safe, community-based care — a scalable model for system-level change.
Speaker: Dr. Saleh Fares Al-Ali (IFEM president)
EMS Global Challenges and Opportunities
Emergency Medical Services (EMS) cannot afford to remain stuck in outdated structures and legacy thinking. In this powerful talk, the speaker called for a bold rethink of EMS models, urging the global community to break down silos, modernize systems, and recognize EMS as a critical component of public health infrastructure — not a standalone service.
🐴 The Dead Horse Theory: Time to Dismount
Legacy EMS systems often rely on inefficient or outdated frameworks, even when evidence shows they no longer serve patients or providers. The “Dead Horse Theory” — the tendency to keep riding a failing system rather than change direction — was used as a central metaphor to emphasize the urgent need for innovation.
🔗 Integration, Not Isolation
A core message: prehospital care must be integrated with hospital services and positioned within a broader health emergency management model.
Key takeaways:
EMS should not function in isolation — it is a key pillar of public health
Stronger collaboration is needed between EMS, EDs, public health, and community systems
Rethinking structures will allow for faster response, better patient outcomes, and more resilient systems
🌍 A Call for Global Coordination
The speaker proposed the formation of an International Prehospital Care Federation — a collaborative global body that could:
Align prehospital care standards and priorities
Facilitate international partnerships
Collaborate with IFEM and other global emergency medicine organizations
Support existing efforts, such as the new Emergency Nursing Federation
💬 “Emergency care is global — our coordination should be too.”
Final Thought
If we want EMS to meet the demands of the future, we must stop reviving the dead horse and start building systems that reflect today’s realities. The time for siloed thinking is over. The future of EMS is interconnected, integrated, and international.
Hardcore EM, Just the Facts: Rapid-fire sessions delivered concise, evidence-based updates on critical emergency medicine topics.
Speaker: Dr. Laurie Morrison
What’s changing in resuscitation guidelines for 2025? Here’s a rapid-fire rundown:
Dr. Laurie Morrison presented high-impact updates on the future direction of resuscitation care, grounded in upcoming ILCOR recommendations and emerging evidence. Here are the most critical takeaways for emergency clinicians:
Mechanical Circulatory Support (MCS) After ROSC
ILCOR: MCS is not superior to standard care post-ROSC in cardiac arrest.
Consider when high-quality manual CPR is not feasible.
In STEMI + cardiogenic shock, MCS still has a role.
Double Sequential External Defibrillation (DSED)
Use DSED for refractory VF after three shocks.
Combining vector change with double sequential defibrillation improves survival to discharge.
Only DSED, not vector change alone, improves functional survival.
Vascular Access: IV vs IO
ILCOR: Start with IV access.
Proceed to IO only after two failed IV attempts.
Hyperkalemia in Pediatric Arrest
ILCOR-supported interventions:
Insulin + glucose
Beta-2 agonists (IV or inhaled)
Bicarbonate has no role in adult hyperkalemia.
Calcium and bicarbonate lack strong evidence in pediatrics.
Layperson Chest Compressions
ILCOR: Strong recommendation to "push deep, push hard"
Minimal risk of injury from bystander compressions in non-arrest patients
CPR Coaching
Recommend including a CPR coach during both adult and pediatric cardiac arrests
Effective if staffing allows, improves rhythm recognition and performance
Looking Forward: Beyond ROSC
Survival to hospital discharge has plateaued. The future of resuscitation must focus on functional survival, shifting emphasis to preserving brain and lung function post-arrest.
Summary
ILCOR’s 2025 updates reflect a move toward more tailored, physiologically grounded care. Emergency clinicians should embrace tools like DSED, reassess IV/IO strategies, and broaden focus to the quality of survival, not just ROSC.
Speaker: Dr. Ffion Davies
Sudden Arrhythmia Death Syndrome
Sudden cardiac death in the young remains a rare but profoundly tragic event. During a recent week in the UK, 12 young individuals died suddenly, underscoring the importance of early recognition and prevention strategies.
Who Is at Risk?
Young athletes are particularly vulnerable. Football players are at increased risk due to sustained exertional tachycardia, while basketball players—especially Black males—are at higher risk due to genetic predispositions to cardiomyopathies.
Warning Signs and Red Flags
Clinicians should ask the same key questions used in elderly patients when assessing young individuals:
What happened before, during, and after the event?
Is there any history of unexplained syncope?
Is there a family history of sudden cardiac death at a young age?
Obtaining an ECG is essential. While over 80% of causes of sudden arrhythmic death can be detected with ECG, the test is not sensitive enough to rule out all potential issues.
Underlying Causes
Sudden arrhythmic death in the young can be divided into three main categories:
1. Structural Abnormalities
Hypertrophic Obstructive Cardiomyopathy (HOCM): Develops over time, resulting in left ventricular outflow tract (LVOT) obstruction, stiff ventricles, and fibroplasia. ECG findings may include deep inverted T waves, q-waves, and large amplitude R/S waves.
Arrhythmogenic Cardiomyopathy: A genetic disorder often affecting the right ventricle.
2. Conduction Abnormalities
Wolff-Parkinson-White Syndrome (WPW): Characterized by a short PR interval and delta wave on ECG, predisposing to reentrant arrhythmias.
3. Ion Channelopathies
Long QT and Short QT Syndromes: These predispose patients to dangerous ventricular arrhythmias.
Brugada Syndrome: Often silent on resting ECG and may only appear with triggers like fever or exercise.
Catecholaminergic Polymorphic Ventricular Tachycardia (CPVT): Triggered by adrenergic stimulation, leading to polymorphic VT.
Clinical Takeaway
Sudden arrhythmic death in the young is often preventable. A high index of suspicion, careful history-taking, and early ECG can lead to timely diagnosis and intervention. Do not underestimate fainting or a positive family history—these red flags can be lifesaving.
Speaker: Dr. Paul Olszynski
Go with the Flow: High Yield PoCUS Applications that Will Improve Departmental Flow
Point-of-care ultrasound (POCUS) isn’t just a diagnostic tool — it’s a strategic intervention that can directly impact departmental efficiency and patient flow. In this high-yield session, Dr. Paul Olszynski emphasized the role of POCUS in streamlining care for common emergency department presentations, with a focus on how likelihood ratios (LRs) guide its utility in low pre-test probability settings.
Why POCUS Improves Flow
Using the principles of Bayes’ Theorem and the Fagan Nomogram, Dr. Olszynski reminded us that POCUS is most impactful when the pre-test probability of a condition is low to intermediate. In these situations, a well-performed bedside ultrasound can either confidently rule out pathology or rapidly escalate the diagnostic pathway.
Clinical Scenarios
1. Swollen Leg: DVT or Cellulitis?
A frequent diagnostic dilemma — is that leg swelling due to a clot or an infection?
POCUS for DVT:
Positive LR: 12.7
Negative LR: 0.12
🧠 Interpretation:
An excellent test for both ruling in and ruling out DVT. A negative scan in a low-risk patient can often eliminate the need for further imaging.
2. Flank Pain: Renal Colic?
A classic renal colic presentation often gets delayed by imaging backlogs.
POCUS for hydronephrosis:
Positive LR: 2.5
Negative LR: 0.16
🧠 Interpretation:
While not definitive, bedside ultrasound showing hydronephrosis increases your diagnostic confidence, and a negative scan is helpful in lower-risk patients.
3. Nausea, Vomiting, and Abdominal Pain: Gallstones or Gastritis?
A frequent ED scenario where quick answers change everything.
POCUS for Cholelithiasis:
Positive LR: 15.5
Negative LR: 0.07
🧠 Interpretation:
This is where POCUS truly shines — the presence of gallstones with a compatible story can help expedite surgical consults and reduce length of stay.
Take-Home Points
✔️ Use POCUS when pre-test probability is low–intermediate
✔️ Know your likelihood ratios — they’re what make your scan useful
✔️ Fast answers reduce unnecessary imaging, improve disposition decisions, and enhance flow
💡 Bottom Line:
POCUS = better decisions, faster. Not just for critical care — it’s a department-wide accelerator.
Lighting Orals: Just the Pearls from some of the latest research in the Emergency Medicine world.
Research in EM Education
Speaker: Dr. Sebastian Dewhirst
Title: Entrustment-Supervision Scales Change Assessor Behaviour
Dr. Sebastian Dewhirst presented compelling evidence that the tools we use to assess trainees may influence more than just the scores — they may actually change the behaviour of assessors themselves.
The study focused on the concept of assessor leniency, a well-recognized phenomenon where some supervisors consistently give higher or lower scores, regardless of the actual performance of the trainee. This trait tends to be stable over time and difficult to influence.
Dr. Dewhirst’s team introduced an Entrustment-Supervision (ES) scale to determine if the structure of the assessment tool could alter these entrenched tendencies. The results were striking — after transitioning to the ES scale, they observed:
A significant change in assessor behaviour
Reduced variability in trainee scores
A dampening effect on leniency and stringency, leading to more consistent, reliable evaluations
These findings challenge previous assumptions that assessment tools are neutral. Instead, they suggest that thoughtfully designed assessment frameworks like the ES scale may help mitigate evaluator bias, contributing to fairer and more accurate assessments of learner performance.
Bottom Line:
Adopting entrustment-based assessment tools can not only improve the fidelity of trainee evaluations but also reshape assessor habits and reduce bias in medical education.
Speaker: Dr. Colin Evans
Title: Evaluating the integration of team cognition training and evaluation in Canadian emergency medicine simulation training (LO50)
Dr. Colin Evans delivered a thoughtful exploration of how Canadian simulation educators conceptualize, teach, and assess team cognition — the shared understanding that underpins effective team performance in acute care settings.
Team cognition in emergency medicine is often described using terms like team situational awareness or team mental models. While these concepts are widely referenced in training and simulation, their practical implementation varies significantly across programs.
Using a constructivist qualitative approach, Dr. Evans and colleagues interviewed simulation leads across 18 programs. Four key themes emerged:
“We’re not there yet”
Many programs struggle with limited resources, inconsistent faculty training, and a lack of protected time to implement non-technical skill training. The result is uneven delivery of team-based learning.
Infidelity in Simulation
Simulations often involve groups of residents, not true interprofessional teams, limiting the authenticity needed to cultivate or assess team cognition.
Recognition vs Misapplication
Educators generally recognize team cognition terminology, but there is confusion around its proper use. Key concepts from human factors literature are often misapplied or conflated.
The Safe Space Dilemma
There’s widespread hesitation to assess team performance due to the belief that simulation must remain a psychologically safe “no-stakes” environment. However, Dr. Evans argues that formative assessment can enhance, not undermine, that safety when done properly.
Interestingly, one program stood apart — a well-resourced, simulation-led institution with rigorous training, standardized terminology, and a clear framework for assessing non-technical skills. This example suggests that excellence is possible with the right support and structure.
Bottom Line:
Simulation programs across Canada show great promise, but there is still a long road ahead in effectively teaching and assessing team cognition. More clarity, resources, and deliberate structure are needed to move the field forward.
Speaker: Dr. Naman Arora
Title: Growth or Performance? Understanding Perceptions of EPA Assessments in Emergency Medicine
Summary:
Since the 2017 introduction of Competency by Design in Canadian medical education, EPAs (Entrustable Professional Activities) have become a cornerstone of assessment. These tools aim to support both assessment for learning (growth) and assessment of learning (performance). However, many critics argue EPAs function more like checkboxes than catalysts for development.
Dr. Naman Arora’s team set out to understand how EPAs are truly perceived in practice: do faculty and residents see them as growth-focused, performance-focused, or somewhere in between?
Key Findings:
Residents viewed 41% of assessments as growth-focused, 30% as performance-focused, and 28% as balanced
Attendings showed a similar distribution
There was moderate agreement between resident and attending perceptions
Pre-assessment factors (e.g., case difficulty, resident mindset, training level, goal-setting) shaped perception before the interaction even began
Only two in-the-moment factors influenced perception: the rationale for triggering the EPA and whether future growth was discussed
Insight:
Faculty-triggered EPAs and conversations about future development were more likely to result in growth-focused experiences, even for senior trainees. A small shift in intention and language made a big difference in how assessments were perceived.
Bottom Line:
EPA assessments can be meaningful, growth-oriented experiences — but it takes deliberate effort. Faculty development and cultural change are key to aligning assessment practices with the goals of Competency by Design.
Rural Emergency Medicine: Talks explored the unique challenges and innovations in delivering high-quality emergency care in rural and remote settings.
Rural Emergency Medicine: Different, Not Deficient
Rural emergency departments aren’t a diluted version of care — they’re a distinct, demanding, and vital part of the healthcare system. That was the resounding message from a powerhouse panel moderated by Drs. Richard Fleet (Canada) and Tim Baker (Australia), with speakers representing rural EM expertise from Canada, Australia, New Zealand, the UK, France, and the US.
Myth-Busting the Rural Narrative
Dr. Sean Moore and Dr. Sally McCarthy tackled one of the most damaging misconceptions: that rural EM is somehow “less.”
💬 “Either I do know what I’m talking about and you have to take the patient, or I don’t—and you still have to take the patient.”
This frustration—of being second-guessed because of geography—is common. But the reality is clear: rural clinicians are generalists with broad expertise, practicing with autonomy and clinical courage.
Innovation Looks Different Here
In rural EM, innovation often grows from necessity:
Ornge (Canada): Bringing care to the patient, not just the patient to care
New Brunswick: Virtual overnight coverage to preserve on-site clinician bandwidth and rest
Allied Health Integration: Home visits and direct paramedic referrals to reduce unnecessary ED visits
These aren’t flashy fixes — they’re community-driven, sustainable solutions.
Who Belongs in Rural EM?
There’s no checklist, but common threads include:
A passion for people and place
Early exposure to rural rotations
And above all, clinical courage — the willingness to act when no one else is there
What Is Clinical Courage?
It’s making the hard call with no backup.
It’s staying when others transfer.
It’s advocating for your patient, even when the system says no.
Clinical courage is what makes rural EM different — not deficient.
Looking Forward
We need:
Training programs that prepare learners for rural realities
Policy and leadership pathways that support rural clinicians
A renewed respect for the value of generalists
💬 “If you believe in rural healthcare and equity, take the lead. If you don’t do it, no one will.”
Rural EM is one of the best jobs in medicine — rich in procedural variety, cognitive challenge, and human connection. And it’s where leadership and impact aren’t just possible — they’re essential.
⚕️ Afternoon Plenary: Saving Emergency Medicine - A Global Perspective on Current Challenges and Potential Solutions
Speakers: Dr's. Paul Atkinson, Ffion Davies, Salah Fares Al-Ali and Modearted by Dr. Eillyne Seow
“Saving Emergency Medicine” 🩺💬
Dr. Paul Atkinson (@paulatkinsonem) reminds us that compassion isn’t a soft skill — it’s core to how we survive and sustain emergency care.
🧠 Emergency medicine is not failing because we don’t care — it’s failing because we’re working in broken systems. Click here for a longer breakdown of his conversation and practical tips to help improve your compassion.
Dr. Ffion Davies reminds us that thriving in emergency medicine isn’t about resilience alone — it’s about systems and culture that prioritize basic human needs, strong leadership, and individual control. Burnout is real, but so is the potential to thrive. Dr. Ffion Davies shared key insights into what actually sustains emergency physicians and staff in high-stress environments.
1. Your Basic Needs Must Be Met
It sounds simple, but it’s often overlooked. You cannot thrive if you can’t meet your most basic physiological and psychological needs. Ask yourself:
Can you take breaks during your shift?
Do you have easy access to bathrooms, food, water, and a quiet space?
Do you feel safe getting to and from work, and while you’re there?
📌 Key message: Safety and self-care are foundational, not optional.
2. You Need Someone Fighting for Good
Great leaders make all the difference. Not because they fix every problem, but because they make people feel seen, supported, and valued.
Leadership should focus on fulfilling three core human needs:
Competence – “I’m good at what I do.”
Autonomy – “I have a say in how I do it.”
Relatedness – “I’m part of something bigger than myself.”
📌 Strong leadership doesn’t just guide – it protects.
3. A Sense of Control Over Your Destiny
One practical example? Self-rostering.
Allowing clinicians to contribute to their schedules gives them a sense of ownership over their time, improves work-life balance, and can significantly reduce stress.
📌 Agency is one of the most protective factors against burnout.
Final Thoughts
Thriving in emergency medicine doesn’t require superhuman endurance. It requires:
✅ Systems that support staff
✅ Leaders who advocate and listen
✅ Environments that promote control, connection, and care
🔍 Afternoon Concurrent Tracks 1
Digital EM and Tech Innovation: Sessions explored the integration of digital tools in emergency settings, highlighting advancements in telemedicine, electronic health records, and AI-driven diagnostics.
Speakers: Dr's. Henry Li, Hashim Kareemi, Ilitea Kina, Yih Yng Ng, Gabreille Bunney
What does the everyday emergency physician need to know about artificial intelligence?

Artificial intelligence is already shaping emergency medicine — from triage to documentation. But with growing hype comes the need for clarity, caution, and clinical responsibility. This session broke down what frontline physicians actually need to know about AI, machine learning, large language models, and digital integration.
🧠 Understanding the Types of AI
While AI can be categorized in many technical ways, emergency physicians should focus on three practical domains:
Computer Vision
AI that analyzes images and videos.
Example: Radiograph interpretation, fall detection systems.
Natural Language Processing (NLP)
AI that processes human language.
Example: LLM-powered charting tools, billing support, clinical documentation.
Prediction Modeling
AI that uses historical data to forecast outcomes.
Example: Sepsis alerts, triage prioritization models.
🩺 Clinical Use Cases & Warnings
🔹 Dr. Gabrielle Bunney (Stanford, USA): Predictive Models & ECG Screening
Delayed ECGs mean missed early pathology
ACS patients often mis-triaged at registration
Predictive AI models could flag high-risk cases earlier — especially with ECG and triage data integration
Ethical Considerations
AI in medicine must be handled with care. Key concerns include:
Patient Privacy and Data Security
Especially relevant for third-party apps outside the EHR environment.
Informed Consent
Patients deserve transparency about the use of AI in their care—and its limitations.
Equity and Bias
Models trained on non-representative datasets may perpetuate systemic inequities, particularly across race, ethnicity, and gender.
🔹 Dr. Ili Kina (Alberta, Canada): OpenEvidence & Hallucination Risk
LLMs can hallucinate: Sound confident but be completely wrong
OpenEvidence minimizes this by applying LLMs only to retrieved, cited evidence
Output includes linked references for clinicians to verify
Advice:
Feed the model clear, specific prompts
Maintain critical appraisal
You’re still medico-legally responsible for decisions
🔹 Dr. Henry Li (Toronto, Canada): AI Scribes for Documentation
Documentation burden contributes to clinician burnout
AI scribes offer fast, flexible note-taking:
Conversation → Recording → Transcript → Summary
Faster than traditional scribes, customizable
LLM use here is limited to language tasks, not clinical decision-making — a safer and more immediate application
🔹 Dr. Yih Yng Ng (Singapore): Strategy, Funding & Equity
Demand for AI exceeds current capacity
Clinicians must co-lead AI development and funding decisions
Form AI literacy and policy groups to shape ethical and effective deployment
Sharing code, data, and models across institutions = scale and sustainability
💡 AI is expensive. Collaboration and resource-sharing are key.
Final Takeaways
AI is not a brain replacement — it’s a tool.
Be cautious of “black box” solutions.
Own your data.
Don’t forget: good clinical judgment is not replaceable.
Speakers: Dr's. Jessalyn Holodinsky & Dr. Fareen Zaver
Bias and Ethics in AI: Safeguarding Patient Care in Emergency Medicine
Artificial intelligence is only as fair as the data and assumptions behind it. In this powerful session, Drs. Holodinsky and Zaver explored how bias in AI systems can subtly — and dangerously — influence care in the emergency department. As emergency physicians increasingly adopt AI tools like scribes and triage systems, the need for ethical vigilance has never been greater.
What Is Bias in AI?
Bias refers to any factor that causes an AI system to produce inequitable or inconsistent outputs — particularly across different patient populations. It can arise from:
Training on non-representative datasets (e.g. data skewed toward WEIRD populations: White, Educated, Industrialized, Rich, Democratic)
Missing variables like race, ethnicity, socioeconomic status, or gender identity
Historical patterns of systemic discrimination embedded in the data itself
Case 1: Language and Cultural Barriers
A 55-year-old woman from an ethnic minority background underplayed her symptoms during a clinical encounter. While the clinician was able to interpret nuance and context, the AI scribe struggled — missing subtle information due to a language barrier and lack of cultural awareness.
Case 2: Gender Identity and Clinical Framing
A 28-year-old transgender woman presented with chest pain. The clinician documented a psychosomatic framing, emphasizing hormonal and anxiety-related causes. The AI scribe, however, generated a more neutral and objective summary, without such framing bias.
Final Thoughts
AI doesn’t eliminate bias — it can amplify it unless thoughtfully designed and critically used. For emergency physicians, AI should be:
A tool, not a truth
A prompt for self-reflection, not a replacement for clinical reasoning
Scrutinized for how it handles marginalized populations
As AI continues to expand into emergency medicine, we must stay anchored in equity, ethics, and patient-centered care.
Hardcore EM, Just the Facts: Rapid-fire sessions delivered concise, evidence-based updates on critical emergency medicine topics.
Speaker: Erin O'Conner
When There is Nothing More to be Done
In emergency medicine, we often focus on saving lives. But what about when saving a life isn’t possible? Dr. Erin O’Connor challenges us to rethink our role — not as fixers, but as guides through the most human moments of medicine. When cure is no longer the goal, compassion and clarity become the treatment.
Your Patient is Also Their People
Imagine a patient with end-stage COPD, in severe distress and delirium. Yes — they are your patient. But so is their family, their caregiver, their partner at the bedside. In these cases, the outcome of the discussion is not what matters most — the discussion itself is.
💬 “Why should I have to do this? I’m not their GP or oncologist.”
Because in that moment, you are the one who is there. Your job is to:
Offer clear, honest information
Make a recommendation
Support the family — and release control of the decision
A Simple Framework: Wish, Worry, Wonder
Dr. O’Connor shared a powerful communication tool for goals-of-care conversations:
Wish (acknowledge): “I wish your father didn’t have to be here.”
Worry (state the facts): “I worry that if we intubate, he may never leave the ICU.”
Wonder (make a recommendation): “I wonder if we should focus on comfort and medical management.”
Use Concrete Language
✔ Say:
“Death and dying”
“Allow a natural end of life”
“This must be incredibly hard”
✖ Avoid:
“I know how you feel”
“Let them go”
“Pass away”
Symptom Management Isn’t a Checklist
Each patient is different. Dr. O’Connor emphasized thoughtful, individualized care:
Dyspnea
Non-medical: Raise HOB, fan to face
Morphine 1–2 mg IV/SC q30min PRN
2nd line: Lorazepam 0.5–2 mg SL/IV/SC
Delirium
Dim lights, silence alarms
Haldol 0.5–2 mg PO/SC/IV
2nd line: Lorazepam 0.5–2 mg
Secretions (Death Rattle)
Stop IV fluids
Avoid suctioning
Glycopyrrolate 0.2–0.4 mg SC q4h PRN
Scopolamine 0.4 mg SC q4h PRN
Pain
New to opioids: Morphine or Dilaudid
Severe: Ketamine 0.3–0.5 mg/kg IV
Already on opioids: Convert to IV/SC (PO:IV is 5:1)
Nausea/Vomiting
1st line: Metoclopramide 5–10 mg IV/SC
2nd line: Haldol 0.5 mg q4h PRN
Three Take-Home Messages
Conversation is the goal — not the outcome
Wish, Worry, Wonder
Symptom management isn’t a checklist — it’s personalized care
Speaker: Dr. Sara Crager
The Big 3: Misses that Matter the Most
Emergency medicine is fast, chaotic, and full of high-stakes decisions. But some misses matter more than others — not because they’re common, but because when they go wrong, they’re hard to undo. Dr. Sara Crager shared three critical areas where early ED decisions have lasting downstream consequences.
💬 “Finding the needle in the haystack is only half the battle. How you manage it — that’s what matters.”
🎯 Strategic Focus: What’s Worth Your Time?
Not all “sick” patients are complicated — and not all complicated patients need urgent action in the ED.
The key is to recognize which patients need your focus because what you do (or don’t do) really matters.
1️⃣ Dyspnea: It’s Not Always the Lungs
A tachycardic, diaphoretic patient gasping for air might not have a primary pulmonary problem.
🚫 Intubation won’t fix metabolic acidosis or shock — and might actually make them worse.
Red flags:
Normal BP does NOT rule out severity (compensation masks shock)
Hypercapnia? ARDS? Metabolic acidosis? Intubation may not be the solution
Intubate the wrong dyspneic patient, and you may push them over the edge
2️⃣ Shock = Hypoperfusion, NOT Hypotension
💡 Shock is a spectrum, not a single number.
Compensated shock: Vital signs still look okay, but tissues are underperfused
Decompensated shock: Reserve is gone, and the patient crashes
“Occult shock” = we missed it
How to recognize early shock:
Clinical exam: Mental status, diaphoresis, mottling, cap refill, urine output
Labs: Lactate, base excess, HCO₃, glucose, creatinine, LFTs, INR
Monitoring: HR, temp, RR, waveform analysis, BP trends — not just numbers
3️⃣ Lactate ≠ Sepsis ≠ Fluids
Stop the “lacto-bolus reflex.”
A high lactate isn’t a trigger for blind fluid administration.
Ask instead:
Am I identifying the right type of shock?
Have I fully addressed the shock trigger?
Could multiple types of shock be at play (e.g., septic + cardiogenic)?
💬 “Fluids are medications. Be just as thoughtful with them as you are with antibiotics or sedatives.”
Final Thoughts
In the ED, some decisions reverberate all the way to the ICU — or the morgue.
Dr. Crager’s challenge: Recognize the patients where your actions matter most.
✅ Don’t be fooled by vitals
✅ Look for shock before it looks obvious
✅ Resist reflexive management — and treat the right problem
Speaker: Sara Gray
Status epilepticus: when minutes count. Click here to read more
Equity, Diversity, Inclusivity and Accessibility: Sessions emphasize the urgent need to design emergency care systems that are equitable, inclusive, and responsive to diverse populations — both for patients and providers.
Emergency medicine thrives when it reflects the diversity of the communities it serves. In this powerful dual-panel session, moderated by Dr. Constance LeBlanc, international leaders explored the systemic barriers that persist in healthcare and the strategies needed to dismantle them — from mentorship and sponsorship to leadership access and inclusion by design.
Panel: Ffion Davies, Alan Drummond, Gayle Galletta, Aimee Kernick, Ian Higginson
Different Experiences, Shared Challenges
With perspectives from across the UK, Canada, France, Australia, and the U.S., panellists highlighted a common thread: many inequities in emergency medicine stem not from lack of talent — but from lack of access and opportunity.
Key points raised:
Gender bias continues to impact career progression, with women often overlooked for leadership unless they “feel qualified,” while male colleagues are more likely to accept without hesitation.
Inclusion isn’t just an invitation — it’s active, intentional participation.
Ageism limits younger physicians’ access to leadership roles.
Financial barriers disproportionately affect clinicians from low- and middle-income countries, limiting their ability to attend global meetings or influence policy.
Mentorship vs Sponsorship: Know the Difference
One speaker shared a defining story of joining the IFEM Gender-Specific Issues Special Interest Group, where a male colleague became her sponsor, opening doors and guiding her path to eventually chair the group.
💡 Mentorship offers advice.
💡 Sponsorship opens doors.
“I didn’t even realize I wasn’t being sponsored — until I saw the difference it made.”
The panel endorsed the “30-5-1 pledge” — an idea from J.P. Morgan to close gender gaps in advancement:
30 minutes/month of mentorship
5 minutes of vocal recognition
1 minute of public amplification
This small monthly investment can create meaningful impact for underrepresented colleagues.
Action, Not Aspiration
The panel emphasized that EDI work is not a side project — it must be embedded into the daily operations, hiring, and leadership practices of emergency medicine.
Attendees were encouraged to:
Reflect on where bias exists in their teams
Be intentional in designing inclusive systems
Sponsor others, not just mentor
Advocate for structural change, not just representation
True equity isn’t about checking a box — it’s about changing the system.
The session ended with open dialogue from attendees around the globe, reinforcing that EDI is not just relevant in one region — it’s essential everywhere.
Rural Emergency Medicine: Talks explored the unique challenges and innovations in delivering high-quality emergency care in rural and remote settings.
Speaker: Dr. Richard Fleet
Living Labs as a Solution to Improve Rural Emergency Care
Rural emergency care is in crisis — with stark disparities in access, resources, and outcomes. But what if the key to solving these challenges lies not just in traditional research pipelines, but in creativity, collaboration, and community-driven innovation?
Dr. Richard Fleet proposes a novel approach: Living Labs — spaces where clinicians, researchers, citizens, and creatives come together to co-design real-world solutions.
Rural vs Urban: The Gap Is Real
In Canada, stroke patients have a 25% higher risk of death in rural hospitals
In Quebec, rural vs urban mortality is over 3x higher
Fewer than 15% of rural sites have access to a CT scanner
💡 And translating research into practice? Still takes 17 years on average.
1️⃣ CIRCUS: Knowledge Transfer, Montreal-Style
Why not get creative?
Montreal, the world capital of circus arts, inspires Dr. Fleet’s first lesson: join the circus.
🧠 “If we want to move ideas faster from research to bedside — we need to engage, entertain, and connect.”
2️⃣ Living Lab Charlevoix: Innovation with Heart
Living Labs bring innovation to life — not in theory, but in real communities, with real users.
🔬 Living Lab Charlevoix is testing:
Mobile ambulances with point-of-care tech
Portable vital signs monitors
A focus on science + happiness + human-centered design
Most innovations fail. And that’s okay.
Key Principles for Building a Living Lab:
Be audacious: Bold ideas spark bold change
Diversity is power: Citizens, clinicians, artists, students, researchers — all have a role
Be patient: Start small, stay focused
Learn the tools: Design thinking is a discipline
Co-create the future: The best solutions come from within the community
Final Thought
Rural health care doesn’t need more reports — it needs living experiments, led by audacity, inclusion, and empathy. Living labs aren’t a magic fix, but they offer something essential: hope, innovation, and action — rooted in the people who need it most.
Speaker: Dr. Frédéric Lemaire
ChatGPT and AI to Better Rural EM
🔑 Key Takeaways:
Cut through the hype: LLMs are statistical tools—not sentient beings. They don’t “hallucinate,” they just reflect the training data.
Know your context: Always ask yourself: What do I know about this topic? and What are the stakes if this is wrong?
Use AI where it shines:
Documentation (EHR + scribe)
Medical education (case creation, simulations, exams)
Communication (email drafts, summaries)
Cognitive co-pilot (debiasing, brainstorming, steelmanning)
Research assistant (literature review, article summaries)
Use with caution in clinical decision-making: High-stakes, low-knowledge scenarios are dangerous with LLMs. Always verify before acting.
We’re living through the most exciting—and frankly, terrifying—technological shift since the birth of the internet. Large Language Models (LLMs) like ChatGPT are flooding into healthcare, and rural emergency medicine may stand to gain the most… or lose the most, if we’re not careful.
Cutting through the AI buzzwords we ask a simple question: Where can AI genuinely support clinicians in rural settings—and where can it dangerously fail?
🔍 What AI is (and isn’t)
LLMs don’t “hallucinate”—they generate predictions based on massive datasets. They don’t know or understand anything. They’re tools, not oracles.
✅ Where ChatGPT shines:
Documentation: AI scribes can save hours of charting time.
Education: Sim case creation, quiz generation, even full slide decks on topics you already know.
Communication: Meeting notes, patient letters, email drafts.
Cognitive Copilot: Need a fresh take? Use LLMs to steel-man opposing views or reflect on tough cases.
Research Assistant: Initial article triage, summaries, and lit reviews.
🚫 Where it’s dangerous:
When you don’t know much about the subject, but the stakes are high. This is the most dangerous use case—LLMs can give confidently wrong answers. And they’ll say it so smoothly you might just believe them.
💡 Bottom line:
AI won’t replace rural EM docs. But docs who use AI well may outpace those who don’t. Learn its strengths. Respect its limits. And never trust it blindly in clinical care.
Speaker: Dr. Kylie Booth and Dr. Eilieen Cheung
Ontario Health's Peer-to-Peer Program
Two Ontario-based initiatives are transforming emergency medicine practice by fostering community, confidence, and clinical excellence. Together, the Supplemental Emergency Medicine Experience and Ontario Health’s Peer-to-Peer Program are building a more connected, supported, and prepared emergency workforce — especially for clinicians practicing in underserviced or transitioning environments.
🔹 Peer-to-Peer Support, 24/7
The ED Peer-to-Peer Program connects frontline physicians to experienced ED peers across Ontario — in real time, 24/7.
✅ Available for all EDs and all acuity levels
✅ Supports patient care and clinician confidence
✅ Aligns with the Life and Limb policy and existing consultative models
📞 Call CritiCall Ontario at 1-800-668-HELP and ask for an ED Peer — it’s that simple.
💬 “Sometimes, all we need is a quick call to feel supported, validated, and clinically anchored.”
🔹 The Supplemental Emergency Medicine Experience
This program offers immersive, tailored learning for clinicians — especially those transitioning to rural or remote practice.
Key features include:
Mentorship from expert clinicians
Exposure to high-acuity, high-volume environments
Focused upskilling in advanced EM competencies
💡 Designed to support career transitions and build long-term capacity in rural emergency departments.
📈 Impact at a Glance
Program | Key Benefit | Long-Term Impact |
Peer-to-Peer | Real-time coaching & connection | Stronger, more supported clinical decisions |
Supplemental EM Experience | Hands-on skill development | Greater confidence & competence in underserviced regions |
Together, these programs are bridging the gap between learning and leadership, and building a culture of lifelong emergency medicine scholarship across Ontario.
Medical Education and Lifelong Learning: This track highlights evolving strategies to train, support, and sustain emergency clinicians through all stages of their careers.
Speaker: Dr. Jason Frank
Competency-Based EM Training: A Global View
Emergency medicine demands rapid decision-making, high-volume clinical exposure, and real-time teaching — making it the ideal environment for competency-based medical education (CBME). As CBME is increasingly adopted around the world, the focus is shifting from time spent to skills demonstrated — for the benefit of both learners and patients.
Why CBME Fits Emergency Medicine
Dr. Frank argues that traditional, time-based training leads to variability in outcomes — not all graduates are equally prepared. In contrast, CBME emphasizes outcomes, accountability, and tailored progression.
Key advantages of CBME in EM:
Direct observation and real-time feedback
A naturally high caseload across all acuity levels
Graduated responsibility and supervision
Focus on what learners can actually do, not just how long they’ve trained
💬 “Competency-based education aligns with what emergency medicine already values: performance under pressure and growth through challenge.”
Global Momentum, Local Challenges
CBME is now being adopted in training programs worldwide — but significant work remains:
Defining core competencies specific to emergency medicine
Aligning assessment tools across systems and cultures
Ensuring faculty development to support meaningful observation and coaching
Final Thought
Time doesn’t guarantee readiness. Competence does.
The future of emergency medicine training lies in designing systems that prepare physicians to thrive in the chaos — and ensure patients are cared for by clinicians who are truly ready.
Speaker: Dr. Jeffrey Landreville
Coaching in Emergency Medicine, Taking Your Clinical Supervision to the Next Level - Click here to read more
Resuscitation, Trauma and Critical Care: Cutting-edge updates on high-stakes resuscitation, advanced trauma management, and critical care delivery.
Speaker: Dr. Amal Mattu
What's the Latest in Emergency Electrocardiography?
Some of the deadliest coronary occlusions don’t look like STEMIs — and current guidelines may not catch them. Two critical ECG patterns that require emergent reperfusion therapy (ART) are the De Winter T wave pattern and the Aslanger pattern. Recognizing them can save lives — even though they’re not yet in cardiology guidelines.
🔥 The 2022 ACC Decision Pathway — and Its Gaps
While the ACC’s 2022 Expert Consensus outlines criteria for acute reperfusion therapy, it misses key high-risk ECG patterns that require urgent recognition.
🚨 De Winter T Waves
A STEMI equivalent for proximal LAD occlusion
ECG Features:
Upsloping ST depression at the J-point in V2–V4
Tall, symmetric T waves in the same leads
Often with symptoms of ischemia
💡 Pearl: These patients are always symptomatic, and often misdiagnosed.
📍 Key mimic: Hyperkalemia (but hyperK often shows a rightward axis, diffuse ST changes).
🛑 Requires immediate ART – don’t wait for guideline updates.
🚨 Aslanger Pattern
A high-risk STEMI equivalent indicating RCA or LCx occlusion
ECG Features:
STE in lead III only, not in II or aVF
ST in V1 higher than in V2
ST depression in V4–V6 with terminally positive T waves
🧠 Leads III and V1 are contiguous in 3D — a subtle but important clue.
🛑 Requires immediate ART – despite being unrecognized in most guidelines.
If it looks dangerous, treat it like a STEMI, even if the ECG doesn’t meet textbook criteria.
Stay sharp. Stay suspicious. Recognize patterns before the guidelines do.
— Dr. Amal Mattu
Dr. Mattu's slides can be found here for the next 30 days.
Speaker: Dr. Zaffer Qasim
Whole Blood: More than the Sum of its Parts
Traditional blood banking practices involve fractionating donated blood into packed red blood cells (PRBCs), platelets, and plasma — an approach that may be suboptimal for bleeding trauma patients.
Military literature has consistently shown a survival advantage with whole blood compared to component therapy in trauma resuscitation.
Recent civilian data is now echoing these findings. A multicenter trial involving trauma centers in the US and Canada (JAMA Surgery, 2023) demonstrated that adding whole blood to massive transfusion protocols resulted in both early and sustained survival benefits.
Cold-stored whole blood remains viable for up to 35 days when preserved appropriately.
It is also increasingly being used in the prehospital setting, where early results suggest a potential benefit in trauma outcomes.
The risks associated with whole blood transfusion are comparable to those of standard component therapy, and trauma literature indicates these risks are minimal.
Speakers: Dr. Steven Skitch and Sameer Sharif
Critical Decisions in Post-Intubation Management: Best Practices for Ventilation and Sedation in the ED
Post-intubation care doesn’t stop at the tube.
Effective ventilation and timely, tailored sedation are critical to prevent complications, including patient awareness, delirium, and long-term morbidity. This session delivered essential reminders and practical pearls to optimize early post-intubation management in the ED.
🔹 Ventilation: Protect the Lung Early
Lung-protective ventilation (LPV) in the ED has been shown to reduce mortality and pulmonary complications — but only when done correctly and early.
Key Targets:
Tidal volume (Vt): 6 mL/kg ideal body weight (IBW)
FiO₂: Start at 100% and titrate down
Pplat / Ppeak: Keep < 30 cm H₂O
💡 Clinical Pearl: Set LPV from the start — don’t wait for the ICU to do it.
🔹 Sedation: Early, Tailored, and Light
A delay in analgesia or sedation after paralysis increases the risk of awareness in the ED — a preventable harm.
Best Practices:
Initiate sedation immediately after intubation
Assess for pain first, and treat it
Use validated sedation scales to titrate to target
Avoid benzodiazepines (unless specifically indicated)
🔹 Choosing the Right Agents
🟢 Opioids
✅ Excellent analgesia and blunts sympathetic response
⚠️ Risk of accumulation, tolerance, and delirium, especially with continuous infusions
🟢 Ketamine
✅ Dual action: analgesia + sedation
✅ Bronchodilator effect
⚠️ Limited data for continuous post-intubation use
🔴 Midazolam
⚠️ Prolonged sedation and accumulation
⚠️ Avoid continuous infusion when possible
Final Thought
The moments after intubation are critical for setting the trajectory of your patient’s ICU course. Treat pain, titrate sedation carefully, and protect the lungs early — because the ICU starts in the ED.
🔍 Afternoon Concurrent Tracks 2
International and Global Emergency Medicine: Global collaboration and innovation in emergency care delivery, with a focus on health system strengthening, disaster response, and advancing equity across diverse international contexts.
Speaker: Dr. Tushara Suprapaneni
A Spatial Approach to Addressing Humanitarian Crises
In the face of complex humanitarian emergencies, we often turn to boots-on-the-ground coordination, supply chains, and logistics. But what if we could see the crisis more clearly—through data? Dr. Tushara Suprapaneni invites us to consider a powerful tool for emergency response: Geographic Information Systems (GIS).
📍 What Is GIS and Why Does It Matter?
GIS is software that integrates multiple data layers—geography, infrastructure, environment, population demographics, and health systems—to produce interactive, informative maps. These maps help decision-makers understand where help is needed most, how best to deploy resources, and what barriers exist on the ground.
🧭 Applications in Humanitarian Settings
GIS technology is being used across global crises for preparedness and response, including:
Cyclone Idai in Mozambique
Mapping pre- and post-disaster access to healthcare facilities.
Humanitarian presence in Afghanistan
WHO’s “Who, What, Where” (WWW) database maps operational aid efforts across the country.
This spatial understanding enables real-time awareness and smarter interventions when every minute counts.
⚠️ Field Challenges
Despite its promise, GIS implementation isn’t without obstacles:
Data Gaps: Pre-existing datasets may be outdated, incomplete, or non-standardized.
Data Collection Ethics: In humanitarian crises, obtaining informed consent and maintaining data privacy remains complex.
Duplication: In the scramble for visibility, multiple agencies may release overlapping maps that clutter decision-making rather than clarify it.
💡 Bottom Line
GIS offers a data-driven, scalable, and analytically powerful approach to managing humanitarian emergencies. When used thoughtfully, it can improve health equity, guide timely resource allocation, and empower local response efforts.
In crisis settings, a map isn’t just a map—it’s a lifeline.
Speaker: Dr. Nilanka Mudithakumara
A Trainee's Journey in EM
International Emergency Medicine is a welcoming, inclusive space. Through the efforts of the International Federation of Emergency Medicine (IFEM) and global EM leaders, trainees - especially those from low- and middle-income countries (LMICs) are supported and empowered to participate on the world stage.
There are no barriers based on gender or geography. As a female trainee from Sri Lanka, I found an equal seat at the table.
IFEM fosters growth, connection, and leadership development, especially for those driven by purpose and collaboration.
IFEM: A Pathway for Emerging Leaders
One of the most meaningful opportunities came through the IFEM Leadership & Advocacy Development Program, which intentionally seeks out and nurtures emerging leaders—especially from LMICs. Their mentorship and training have been instrumental in shaping my growth.
Additionally, IFEM Special Interest Groups (SIGs) offered an incredible platform for global networking, allowing me to collaborate with mentors and peers from across the world. These networks have not only helped shape my professional journey but have also reaffirmed a personal mission to contribute back to the global EM community.
Hardcore EM, Just the Facts: Rapid-fire sessions delivered concise, evidence-based updates on critical emergency medicine topics.
Speaker: Dr. Simon Carley
Trauma Update
🔹 Resuscitative Hysterotomy: Act Fast to Save the Neonate
Leech et al, Resuscitation 2025
Maternal survival is rare, but neonatal survival is possible—even with prolonged CPR.
If you’re thinking about doing it, you should already be doing it.
💡 Takeaway: Prepare, simulate, and act early in maternal cardiac arrest.
🔹 PECARN C-Spine Rule: Less Imaging, Same Safety
Leonard et al, Lancet Child Adolesc Health 2024
Validated tool with 94% sensitivity and 99.9% NPV.
Can reduce pediatric CT scans by half.
💡 Takeaway: Paediatric-specific rules can reduce unnecessary imaging safely.
🔹 TRAUMOX2: Oxygen Isn’t Always a Lifesaver
Arleth et al, JAMA 2025
No benefit to liberal oxygen targets in trauma patients.
Restrictive SpO₂ (~94%) is safe and reduces atelectasis.
💡 Takeaway: Be deliberate with oxygen—more isn’t better.
🔹 CRYOSTAT-2 & Fibrinogen: Empiric Dosing Falls Short
Davenport et al, JAMA 2023
Early cryoprecipitate did not improve mortality.
Targeted use based on testing is preferred.
💡 Takeaway: Don’t give fibrinogen without knowing the level.
🔹 Prehospital Partial REBOA: Feasible and Promising
Lendrum et al, JAMA Surg 2024
Partial REBOA raised BP in critical patients, 2 survived to discharge.
💡 Takeaway: With training and system readiness, REBOA works prehospital.
🔹 SABRE Trial: SAP Blocks for Rib Fractures
Partyka et al, JAMA Surg 2024
Improved pain, less opioid use—even in posterior fractures.
💡 Takeaway: Ultrasound-guided serratus blocks should be routine.
🔹 Prehospital Thoracotomy: Rare but Not Futile
Perkins et al, JAMA Surg 2025
21% survival in tamponade from penetrating trauma.
No survivors in blunt trauma >15 min of arrest.
💡 Takeaway: Prehospital RT is justified in select penetrating trauma.
🔹 NIBP Inaccuracy in Trauma
Perera et al, Scand J Trauma 2024
NIBP misestimates MAP at physiologic extremes.
💡 Takeaway: Use IBP if BP guides management—especially in TBI or shock.
🔹 HEMOTION: Restrictive Transfusion in TBI
Turgeon et al, NEJM 2024
No benefit from liberal transfusion; more ARDS.
💡 Takeaway: Restrictive strategy (Hb ≤7) is safe in moderate/severe TBI.
🔹 DSI Beats RSI in Trauma Intubation
Subramanian et al, Resuscitation Plus 2024
Less peri-intubation hypoxia, better first-pass success.
💡 Takeaway: DSI should be part of trauma airway protocols.
🔗 Full analysis and citations: St. Emlyn’s Blog – Trauma Top 10 Papers
Speaker: Dr. Sara Crager
Reframing Shock
You’ve heard—or given—this consult before:
“The patient is still hypotensive after two fluid boluses. PoCUS cardiac function looks good, so we’re starting vasopressors.”
But is that enough?
Why Traditional Shock Teaching Falls Short
We’re classically taught the four buckets of shock: hypovolemic, distributive, cardiogenic, obstructive.
Sounds neat and tidy. But patients don’t always come neatly labeled. In reality, they often have features of more than one type, and trying to shoehorn them into a single category isn’t always clinically helpful.
Some have tried to reframe this with a “pipes, pump, tank” model. That’s a step forward, but still assumes we can plug data into static boxes.
So, what happens when you’ve done all the right things—fluids, ultrasound, categories—and the patient is still in shock?
Welcome to the end of the sidewalk.
A Better Way to Think: Perfusion Pressures
Let’s move away from a blood pressure obsession and toward what really matters: tissue perfusion.
Shock isn’t about hypotension—it’s about hypoperfusion.
But because blood pressure is easy to measure, we’ve made it our north star. “MAP > 65 = patient is fine.” But that’s not always true.
Perfusion happens at the capillary level, and there are three pressures we need to account for:
🔹 Forward Pressure
This is what we usually focus on—MAP, cardiac output, left ventricular function.
It’s your pushing force. But it’s not the whole picture.
🔹 Back Pressure
If forward pressure is your push, back pressure is the resistance—like someone on the other side of a boulder pushing back.
Elevated venous pressures, right heart dysfunction, and venous congestion reduce the net perfusion gradient.
🔹 External Pressure
Now imagine someone sitting on top of the boulder. That’s external pressure—forces from outside the vasculature that impair flow.
Think:
Cardiac tamponade
Tension pneumothorax
Even tissue hydrostatic pressure from massive edema or abdominal compartment syndrome
These external forces reduce effective capillary perfusion—right where oxygen exchange matters most.
The Three-Pressure Framework
This mental model—forward, back, and external pressure—helps you move beyond labels and into physiologic reasoning.
It transforms PoCUS from a binary tool (“good squeeze or not”) into a more nuanced investigation:
Is the pump working?
Is there outflow resistance?
Is something compressing the system?
Bottom Line
Think of shock not as a diagnosis to categorize, but as a problem of pressure gradients:
Between arteries and veins
Between inside and outside the vasculature
Between our comfort zone and where true resuscitation lives
Use this framework to translate bedside data into meaningful action. This isn’t a reinvention of shock physiology—it’s an advanced simplification that finally makes it useful where it matters most: in real-time, with real patients.
Speaker: Arun Sayal
"X-Ray Normal" is Not a Diagnosis
Too often in emergency departments, patients are sent home with the label “soft tissue injury” when their X-rays don’t show a fracture. But as Dr. Arun Sayal emphasized in his ICEM 2025 talk, “normal X-ray” is not a diagnosis—it’s a radiographic observation, and a poor substitute for clinical reasoning.
Missed Injuries, Missed Opportunities
After 12 weeks working in a fracture clinic, Dr. Sayal realized just how flawed our typical approach to “normal X-rays” really is.
📌 CMPA data tells the story:
Most common EM malpractice claims? Missed fractures.
Second most common? Missed hand injuries and lacerations.
The obvious injuries are easy. Our job as emergency clinicians is to catch the subtle findings—the ones that don’t scream at us from the film.
“You wouldn’t discharge a chest pain patient with a normal ECG and troponin as ‘non-cardiac’—so why do we do that with ortho injuries?”
Step Back and Reassess
The process needs a reboot:
Generate pre-test probability: Use your history and physical exam to decide how likely a significant injury is before you see the image.
Post-imaging:
If there’s a clear fracture or dislocation → manage accordingly.
If the X-ray is normal, you haven’t reached a diagnosis—you’ve simply ruled out obvious bony injury.
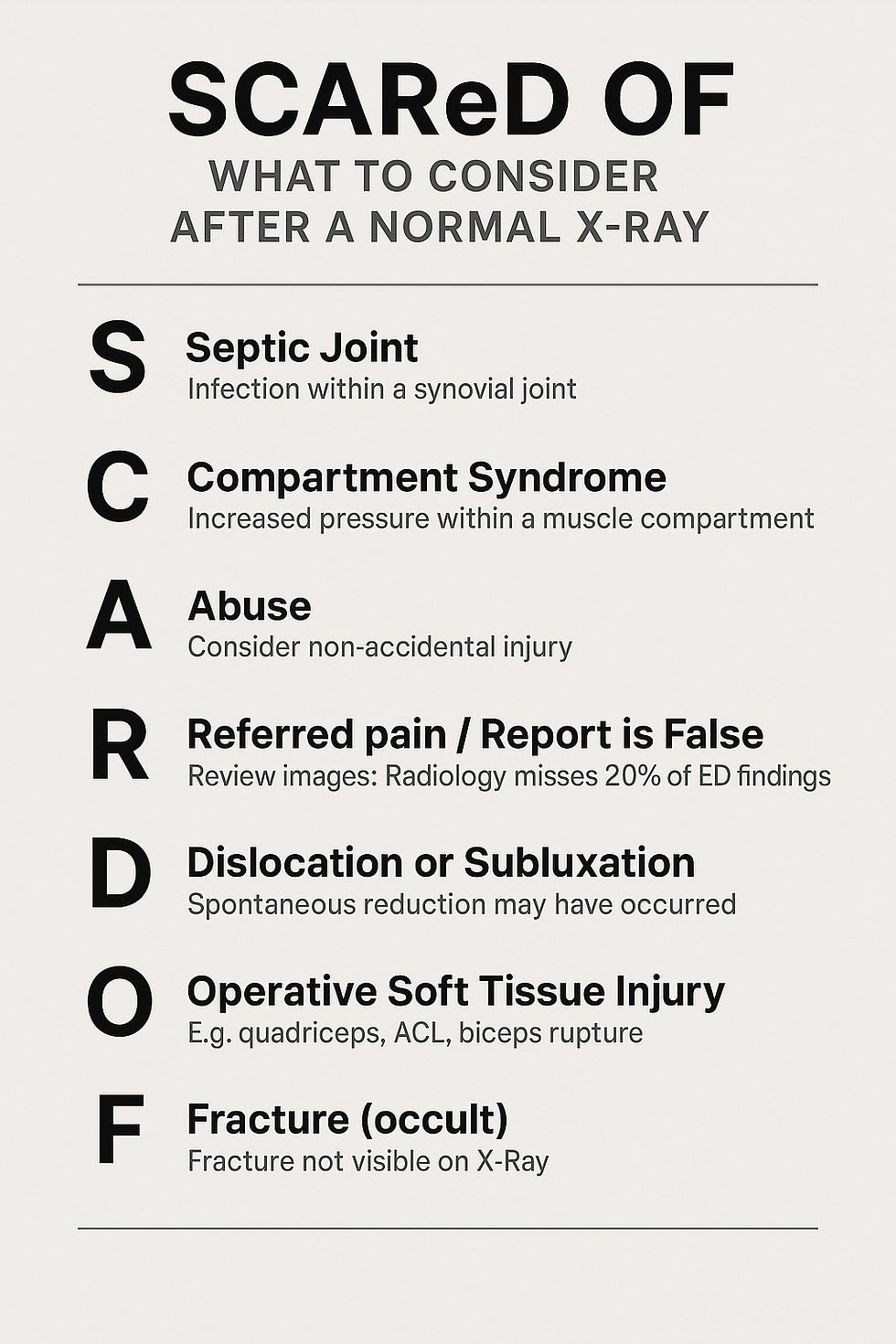
Use the Mnemonic:
SCAReD OF
When the X-ray is unremarkable, ask yourself—what else could this be?
🔍 SCAReD OF is your safety checklist:
S – Septic joint
C – Compartment syndrome
A – Abuse (especially in children or vulnerable adults)
Re – Referred pain or Radiology miss
Radiologists miss ~20% of ED injuries—look at the images yourself
D – Dislocation or subluxation that spontaneously reduced
O – Operative soft tissue injury (e.g. quads rupture, distal biceps, ACL)
F – Fracture (occult and not visible on X-ray—e.g. scaphoid, talus, femoral neck)
Equity, Diversity, Inclusivity and Accessibility: Sessions emphasize the urgent need to design emergency care systems that are equitable, inclusive, and responsive to diverse populations — both for patients and providers.
Speaker: Dr. Sara Gray, Dr. Lindsay MacLean, and Dr. Ayesha Zia
Top 5 Tips for Creating a Women in Emergency Medicine Group (WEM)
Creating a Women in Emergency Medicine (WEM) group is an impactful way to foster community, support equity, and elevate women within the specialty. Here are five practical tips to help you get started, based on our experiences building successful WEM initiatives in Canada.
1. Have a Clear Goal
Start with purpose. Your group needs a defined mission or vision—whether that’s mentorship, career development, networking, advocacy, or wellness. A clear goal helps align your efforts, communicate your value, and measure success. Think: What are we here to achieve?
Pro Tip: Revisit and refine your goal annually as your group evolves.
2. Build Community
A WEM group should be more than a meeting—make it a movement. Foster meaningful relationships through regular events, group chats, social gatherings, or retreats. Prioritize connection over perfection.
Pro Tip: Small efforts (like celebrating promotions or birthdays) go a long way in making members feel seen and valued.
3. Be Inclusive & Engaging
Ensure your space is welcoming to all who identify as women or gender-diverse individuals in emergency medicine. Vary your offerings to include clinical talks, informal dinners, family-friendly events, and virtual options.
Pro Tip: Ask members what they want. Surveys or informal check-ins can guide your programming and make everyone feel included.
4. Mentor, Sponsor & Celebrate
Mentorship is essential, but don’t stop there—be a sponsor too. That means advocating for others behind closed doors. Also, don’t forget to celebrate wins—big and small.
Pro Tip: Create a formal mentorship program or pairing system, and highlight member achievements on social media or newsletters.
5. Get Leadership to Buy-In
Institutional support can elevate your group’s impact. Engage department heads and hospital leadership early. Ask for time, resources, and recognition—this legitimizes your group and opens doors.
Pro Tip: Frame your group as a leadership pipeline or wellness initiative—this aligns with broader institutional goals.
Francophone Track: High yield pearls, presented in French and disseminated in French and English!
Click here to read about the Francophone track in French and English!
Resuscitation, Trauma and Critical Care: Cutting-edge updates on high-stakes resuscitation, advanced trauma management, and critical care delivery.
Speakers: Dr's. Katie Lin and Andrew Petrosoniak
Neurocritical Potpourri
When it comes to crashing neuro patients, the initial moments in the ED are critical. In this practical session, Drs. Katie Lin and Andrew Petrosoniak shared their pearls on how to approach unstable neuro patients, what to prioritize before the CT scanner, and how to optimize early management in stroke and ICH.
1. Crashing Patient: The Focused Neuro Exam
In a critically ill patient with suspected neurological pathology, your neuro exam needs to be rapid and focused. Skip the full neuro exam and concentrate on three key areas:
🔍 GCS Breakdown > Total Score
Don’t just document a number—break it down into Eye (E), Verbal (V), and Motor (M) components.
Especially in the unconscious patient, these distinctions can help clarify brainstem involvement and guide urgency of intervention.
👁 Look at the Eyes
Are the eyes conjugate or disconjugate?
Is there forced gaze deviation?
Test corneal reflexes if deeply unconscious—this can assess brainstem integrity.
💪 Motor Response
Assess for lateralizing signs or lack of movement.
Is the patient localizing, withdrawing, or showing signs of posturing?
🧠 Remember: The focused neuro exam in a crashing brain is:
GCS + Eyes + Motor Strength
2. Secondary Neuroprotection: While You Wait for CT
Even before a definitive diagnosis, early neuroprotective measures can make a major difference.
🛡️ Core Targets
O2 saturation >94%
PCO₂ between 35–40 mmHg
Systolic BP “Safe Zone”: 180–220 mmHg
– Avoid hypotension at all costs!
– Keep the pressure up while you’re still working up the patient
💉 Tips Before CT
Consider antiemetics to prevent vomiting-related spikes in ICP or BP drops from vagal stimulation
If GCS is low or dropping, or there are signs of Cushing’s triad, consider preemptive ICP management:
Elevate head of bed to 30°
Loosen any tight neck ties or cervical collars
Administer 3% hypertonic saline (200 mL)
3. When You Have the Diagnosis
🧠 If CT Shows ICH:
Target SBP <140 mmHg (some suggest 140–160 if concern for hypoperfusion)
Empiric reversal of anticoagulation is recommended if the patient took any anticoagulant in the last 24 hours
→ Go big or go home
🧠 If Acute Ischemic Stroke:
IV thrombolysis if eligible
Endovascular thrombectomy (EVT) if large vessel occlusion (LVO), up to 24 hours from last seen normal
“Wake-up strokes” (patients found with deficits on waking) may perform similarly to early strokes in outcomes and eligibility
4. Four Key Stroke Questions to Ask Every Time
🕒 When were they last seen normal?
🧠 Are the deficits disabling?
🚫 Any contraindications to thrombolysis?
❤️ What’s their goals of care and premorbid status?
✅ Take Home Points
Crashing neuro exam = GCS breakdown + eye movements + strength
Prioritize neuroprotection before CT:
O2 sat > 94%
PCO₂: 35–40 mmHg
SBP:
• ICH: <140
• SAH: <160
• Acute Ischemic Stroke: 185–220 pre-thrombolysis
Don’t delay airway protection if transport or vomiting is a concern
Treat first, scan second — and reverse anticoagulation early if suspected ICH
Speaker: Dr. Ian Stiell
Modern Management of Acute Atrial Fibrillation
Acute atrial fibrillation and flutter can be managed safely and efficiently in the emergency department using evidence-based tools like the CAEP Best Practices Checklist, with rhythm control often being a frontline strategy when the onset is <48 hours.
When is Cardioversion Appropriate?
Acute onset AFib/flutter is typically defined as:
Onset <48 hours ago (or unknown onset if anticoagulated)
First-time or recurrent episode
📍Case Example:
A 67-year-old male presents with 6 hours of palpitations and a history of hypertension. Heart rate is 150.
✔️ This patient would be safe for cardioversion.
❌ If 24 hours had passed without anticoagulation, cardioversion would be deferred due to stroke risk.
What Does the Evidence Say?
🔬 RAFF-2 Trial
Compared drug-shock vs shock-only strategies
Both were safe and effective for acute AFib management
🇨🇦 Canadian Real-World Data
1700 ED cases
90% success rate for cardioversion
18% experienced adverse events (most were minor but required treatment)
Bottom line: Cardioverting in the ED is effective, but you must anticipate and prepare for complications.
📋 The CAEP 2021 Best Practices Checklist
🔗 Read the full checklist here
🧪 RAFF-3 Trial: Checklist Implementation
↓ Length of stay
↑ Cardioversion use
No increase in adverse events
Rate Control Strategies
✅ First-line agents:
Beta-blockers (e.g., metoprolol)
Calcium channel blockers (e.g., diltiazem)
⚠️ Avoid CCBs in heart failure
💡 Digoxin is second-line, but consider as first-line if:
Hypotension
Acute decompensated heart failure
🎯 Target HR: <100 bpm
Rhythm Control Tips
Either pharmacologic or electrical cardioversion is acceptable
Pre-treatment with rate control agents does not improve success
Procainamide is preferred in Canada
❌ Avoid amiodarone in the ED setting (slower onset, less effective acutely)
Electrical Cardioversion Tips
Both anterolateral and anteroposterior pad positions are acceptable
Start with 150–200 joules
Anticoagulation Considerations
Use the CHADS-65 algorithm:
If positive → start anticoagulation in the ED
If negative → consider short-term (4 weeks) anticoagulation
If the patient spontaneously cardioverts, still consider anticoagulation based on risk
🗣 Shared decision-making is key when prescribing OAC at discharge.
Final Thoughts
Modern management of acute atrial fibrillation in the ED is safe, efficient, and evidence-based. The shift toward early rhythm control—especially in patients presenting within 48 hours—has led to higher success rates and shorter ED stays when using structured approaches like the CAEP Best Practices Checklist.
🎉 Thank You for an Incredible Day 2 at ICEM 2025!
As Day 2 of #ICEM2025 wraps up, we extend our heartfelt thanks to all attendees, speakers, and organizers who contributed to another enriching day of learning and connection in Montréal. From dynamic plenary sessions to engaging workshops and thought-provoking discussions, your participation made it memorable.
🎸 Tonight: The Gala & Docs That Rock Concert
The excitement continues tonight with our much-anticipated Gala, starting at 7:00 PM, followed by a high-energy performance by Docs That Rock at 9:00 PM. This unique band of medical professionals is set to deliver an unforgettable evening of music and camaraderie.
📸 Stay Tuned for Highlights
We’ll be sharing photos and highlights from tonight’s festivities in our next daily update. Be sure to check back to relive the moments and see if you can spot yourself in the crowd!
Looking forward to seeing everyone tomorrow for another day of inspiration and collaboration at ICEM 2025!


Comments